 The prevalence, experience and meaning of tooth loss and replacement options have varied historically. In the 1960s approximately 40 percent of UK adults were completely toothless, by 2009 this figure has dropped to 6 percent (National Statistics, Survey, 2009). These lower figures reflect improved oral health care and use of fluoride toothpaste lowering rates of tooth decay. One hundred years ago it was not uncommon to have all your teeth removed as a wedding gift or a 21st birthday present.
The prevalence, experience and meaning of tooth loss and replacement options have varied historically. In the 1960s approximately 40 percent of UK adults were completely toothless, by 2009 this figure has dropped to 6 percent (National Statistics, Survey, 2009). These lower figures reflect improved oral health care and use of fluoride toothpaste lowering rates of tooth decay. One hundred years ago it was not uncommon to have all your teeth removed as a wedding gift or a 21st birthday present.
Currently in the UK, 70 percent of those aged over 75 have a partial denture in one or both jaws, (National Statistics, Survey, 2009) and with the most common causes of tooth loss being gum disease and tooth decay (Petersen , Bourgeois , & Ogawa, 2005 )
What happens to us when we lose teeth?
For those that lose teeth, it can be disabling, and embarrassing. A London based study described individuals’ feeling a sense of grief and bereavement. The shame and moral implications associated with the responsibility of the neglected mouth and oral health problems may be seen as a failure of individual responsibility, rather than that of misfortune. (Fiske , Davis , Frances , & Gelbier , 1998)
This sense of shame, identity shock and profound loss of self-confidence is not noted in other areas of medical rehabilitation, knee or heart valve replacements for example. Even glasses, like dentures that should be removed at night and placed by the bedside do not attract the same shame or stigma. It is also established that people have difficulties accepting tooth loss and experience social avoidance and are perceived as having negative personal characteristics. They are also more likely to experience depression. (Rupal J. Shah, 2015 Jul-Sep) It is clear the main consequence of tooth loss is personal distress.
As far back as 1946, in New York; the World Health Organisation defined health as “Health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity.” Clearly it was recognised that good health was also tightly bound to mental and social wellbeing. That a healthy mouth is a complete and functioning mouth.
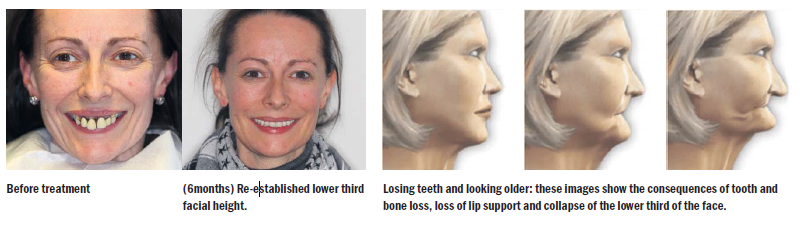
Dentures are seen as a ‘marker’ of old age and removable dentures are perceived as a failure of the self. Our teeth are central to our identity and tooth loss can lead to a disruption and deterioration of self-image. The association between dentures and ageing is one of the powerful motivating factors for people seeking dental implant treatment.
Tooth loss and associated detrimental factors occur over long spans of time. A slow decline in dental health, causes many to be less aware and more accepting of their oral health problems. It’s common to avoid the dentist until pain or problem is no longer bearable. This results in more complex and daunting treatment than should have ever been necessary. This has a negative and compounding effect for visits to the dentist and people can lose hope when faced with such complex conditions and treatment. As a consequence, some feel to have limited options with the teeth they retain, or a denture they struggle with this makes normal life more difficult. These patients are then in the position of neither wanting the teeth they still have nor have any desire for the full dentures on offer.
 What are your options when you lose teeth?
What are your options when you lose teeth?
Until recently, options for replacing missing teeth were relatively limited: partial tooth loss could be replaced with bridges (linked crowns on teeth) or a partial denture (false teeth replacing missing teeth) and those who are toothless, a full denture. Dentures are satisfactory for some patients, whilst others find them difficult to adapt to. Over time, jawbones and gums can shrink, affecting the fit of the denture and causing unwanted movement. This movement causes denture wearers difficulty in use.
 More recently, dental implant treatments have been developed. Allowing replacements of single missing teeth and entire full jaws. These treatments offer patients the option of fixed teeth, with advantages over removable dentures. In the UK dental implant treatment, through the NHS is only available to a very small number of patients with specific clinical need (Royal College of Surgeons Faculty of Dental Surgery, 2019) Most people choosing dental implant treatments will have to pay themselves, substantial personal investment with costs ranging from £5,000 – £20,000 and often more for very complex work.
More recently, dental implant treatments have been developed. Allowing replacements of single missing teeth and entire full jaws. These treatments offer patients the option of fixed teeth, with advantages over removable dentures. In the UK dental implant treatment, through the NHS is only available to a very small number of patients with specific clinical need (Royal College of Surgeons Faculty of Dental Surgery, 2019) Most people choosing dental implant treatments will have to pay themselves, substantial personal investment with costs ranging from £5,000 – £20,000 and often more for very complex work.
Quality of Life improvements following Full Arch Treatment:
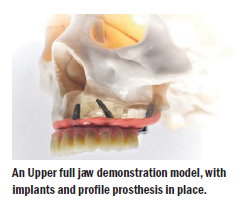
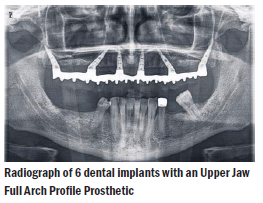
 For those that are suffering severe chronic dental For those that are suffering severe chronic dental disease or where significant tooth loss has occurred, another option now available is to pursue a full mouth rehabilitation. This uses dental implants and a full arch profile prosthesis that replaces the lost teeth, gums and bone structure on either one or both jaws.
For those that are suffering severe chronic dental For those that are suffering severe chronic dental disease or where significant tooth loss has occurred, another option now available is to pursue a full mouth rehabilitation. This uses dental implants and a full arch profile prosthesis that replaces the lost teeth, gums and bone structure on either one or both jaws.
Whilst they have huge potential for a patient, we need to be conscious that ‘forever’ and ‘lifelong’ are aspirational but not always realistic; not in medicine and also not in dentistry. The aim is to significantly extend and improve a patient’s quality of life which may be for some or may be all of an individual’s remaining life. Positively studies evaluating dental related quality of life assessments show the favourable impact they have on a patient’s quality of life (Sargolzaie, 2017).
 Whilst they have huge potential for a patient, we need to be conscious that full arch rehabilitation is a lifelong commitment and involves regular check-ups, and possible repairs and replacements. A dental implant, once integrated and stable for one year after function should last at least 10 years and the prosthetic refurbishment of the implant retained prostheses will need to be considered on average at 10-15 years, although the frequency of this review will depend on patient related factors (Royal College of Surgeons Faculty of Dental Surgery, 2019)
Whilst they have huge potential for a patient, we need to be conscious that full arch rehabilitation is a lifelong commitment and involves regular check-ups, and possible repairs and replacements. A dental implant, once integrated and stable for one year after function should last at least 10 years and the prosthetic refurbishment of the implant retained prostheses will need to be considered on average at 10-15 years, although the frequency of this review will depend on patient related factors (Royal College of Surgeons Faculty of Dental Surgery, 2019)
Full Mouth Rehabilitation – Treatment
Preparation for treatment involves medical dental, psychological, and behavioural risk assessments. The prevention and management of key risk factors for a patient enhances the outcome of treatments. Successful outcome is rooted in shared goals between the patient and the clinical team. The key goal for all is; re-establishment of comfortable and stable chewing and removing disease. Whilst this is not cosmetic treatment, there is a secondary benefit of aesthetics improvement.
The procedure involves placement of dental implants that act as anchors to hold and install a prosthesis that behaves as teeth. Rehabilitations are possible in a day, but post-surgery adaptation and healing periods are much longer. Re-adaptation to a new prosthesis takes time, and whilst the prosthesis can be designed and made to be as comfortable as possible, there is a period of adjustment necessary. On the day of surgery, patients leave with their new fixed teeth and begin the process of healing. Soft diet recommendations are the order of the day for the duration of healing.
Full Mouth Rehabilitation – Post Surgery
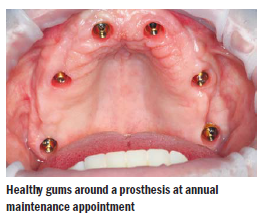
For all patients receiving complex restorative dental treatment, excellent oral hygiene, maintenance recall, and teamwork between the clinical team and patient are mandatory. All dental prosthetics have a biological border. It is the area where the implant connects to the prosthesis and contacts the gums. If gums are left uncleaned, bacteria accumulates and causes irritations to the gums which can lead to a destructive condition known as periodontal disease in the case of implants, peri-implant disease. Cleaning regimes and regular maintenance are of paramount importance.
Full Mouth Rehabilitation – Summary
What are the benefits of fixed full mouth rehabilitation? It is a return to normality for those that feel normal was no longer achievable. It is a final chance at having fixed teeth as an alternative to removable teeth i.e. traditional dentures.