Understanding root canal disease, By Dr William McLean and Dr Sanjeev Bhanderi, The British Endodontic Society
It is estimated that six hundred thousand root canal treatments are performed under the National Health Service each year alone, costing £40 million. For most people, the words ‘root canal treatment’ aren’t the most welcome. To explode the myths surrounding root canal disease, we looked to experts in the field to simplify the terms, explain the basics of root canal and provide some useful knowledge and information to help us understand it better.
Specialists in root canal work are endodontists, one of several types of specialist dentist practitioners who are able to offer a more in-depth service, especially when things are more complicated or need an extra level of experience and expertise.
Root canal treatment is also known as endodontics. The word ‘endodontic’ comes from ‘endo’ meaning inside and ‘odont’ meaning tooth. Like many medical terms, it’s Greek.
WHAT IS ROOT CANAL DISEASE?
It affects the inside of a tooth and is usually caused by bacterial infection. It is treated by disinfection, followed by a root canal filling. The following describes how this diseasepresents and how a dentist may help you keep your tooth.
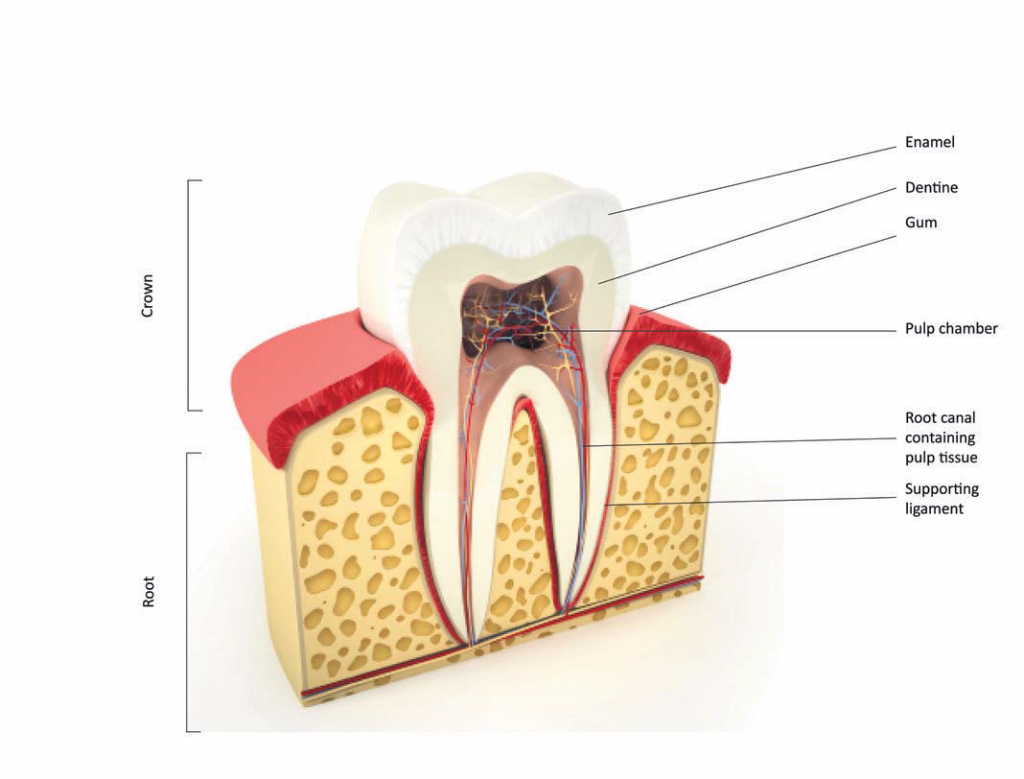
UNDERSTANDING YOUR TOOTH
Your tooth consists of two main parts. The crown, which is that part of the tooth that lies above the gum and is visible in your mouth. Then there’s the root – that part of the tooth that lies beneath the gum and is surrounded by bone. Inside each root is a channel that runs the length of the root and rises into the crown, this is called the root canal. This space contains the pulp (nerves, blood vessels, and soft tissue), often referred to as the ‘nerve’ of
the tooth.
Dental decay, very deep fillings or other dental procedures, a crack in the tooth, trauma, or advanced gum disease can damage the health of the pulp. In some instances the pulp will become inflamed, but recover. If the inflammation is more severe or bacteria are able to penetrate into the pulp it may die and the root canal becomes infected.
SYMPTOMS
An inflamed pulp is often painful and can be triggered or made worse by temperature changes, especially heat. At its worst, pain can occur randomly and lead to disturbance of sleep. When inflammation affects the surrounding bone the tooth may become tender to bite on. Swelling and tenderness in the overlying gums, can also occur. Occasionally, there may be no obvious symptoms.
If an infected root canal is left untreated then the infection can extend beyond the end of the roots and cause inflammation or infection in the surrounding jaw bone.Sometimes this can be quite aggressive and is called a dental abscess. Other times it can slowly and quietly destroy the bone around the tooth, leading to loss of support.
 HOW IS ROOT CANAL DISEASE TREATED?
HOW IS ROOT CANAL DISEASE TREATED?
In order to preserve a tooth that is ‘dying’ or ‘dead’, it is necessary to remove the inflamed pulp or infection from inside the roots to prevent further spread into the surrounding tissues or if already affected allow a return to health. The roots are then filled and sealed. This procedure is known as endodontic or ‘root canal’ therapy and allows the tooth to remain intact and continue to function normally after treatment.
WHO WILL BE ABLE TO HELP YOU?
Your own general dentist will have basic training in endodontics. However, they may decide to refer you to a general dentist with additional training in endodontics or a specialist endodontist. Endodontists are dentists who have been accepted as a General Dental Council registered Specialist in Endodontics – which indicates a recognised level of specialist knowledge and skills.
Who treats you depends on the complexity of the situation. It’s important that the tooth is restored to maximum health, especially if it might be used to support a crown or bridge.
HOW IS ROOT CANAL TREATMENT PERFORMED?
The whole procedure is performed under local anaesthesia so you should not feel any pain. Endodontic therapy should always be performed after the tooth has been isolated by wrapping it up with a protective sheet called a ‘dental dam’ which is secured with a metalclip. This prevents saliva, which contains bacteria, from getting into the tooth during the cleansing procedure and treatment. It also protects you from water, debris and filling materials from falling to the back of your mouth and throat. You can swallow normally and move your tongue around under the dental dam – and the dental nurse has less need to place a suction device into your mouth! It may initially feel a little strange but you will quite quickly feel comfortable and, most importantly, it doesn’t hurt at all.
Endodontic therapy may be performed under an operating microscope or some other form of magnification. Root canals are tiny, and this will give the dentist the best chance of identifying these small spaces. Old fillings and decay will be removed, and then the dentist will explore for all the possible root canals. Once all canals are located, each root canal is carefully cleansed and disinfected right to the natural end of the tooth, and then sealed with a root filling. If the tooth looks too infected at the first visit, or there have been problems in identifying or cleaning all the root canals, your dentists may fill the canals with an antiseptic
dressing and you will need to return for another appointment to complete the rootfilling. The tooth is then restored with a filling to seal the root canal of the tooth and prevent reinfection.
AND AFTERWARDS?
For the first few days after treatment the tooth may feel a little ‘achy’ especially if there was pain or infection before the procedure. This discomfort can be relieved with over the counter or prescription medications. Your dentist may recommend taking an anti-inflammatory just before and after the treatment, or if you have a medical condition that precludes you taking this type of painkiller (e.g. asthma, gastric ulcer), then paracetamol will help. Talk to your dentist about your best solution.
Occasionally, your dentist may want to review the tooth after the root filling has been completed on a 6-monthly basis to monitor your healing response. These appointments are very important as they allow swift intervention if the tooth isn’t responding to treatment. The review appointments are usually quite short and simply involve looking at the tooth and taking an X-ray image to see how well the bone is healing. If you have been treated by a specialist, then they may ask your own general dentist to ‘keep an eye’ on the healing response if it is more convenient for you.
ENDODONTIC MICROSURGERY (‘APICECTOMY’)
Occasionally, conventional root canal treatment (through the top of the tooth) may not work or cannot be performed. Reasons for this include longstanding infection that extends onto the outside of the root surface, blockage of the root canal impeding proper cleaning and the resence of crowns, posts or bridgework that makes access to the root canal complicated.
THE PROCEDURE
The whole procedure will be performed under a surgical microscope. Briefly, anaesthetic will be delivered so the tooth and gum is numb. The overlying gum tissue over the site of the root infection is peeled back so direct access is made to the infected tissue. The tissue is then removed together with the infected root-end. A small root filling is then placed back into the root canal to seal the root, and the gum tissues are stitched back so that they can heal normally. Over the first few weeks the gums will heal back to their normal appearance and over a period of months, the bone will heal round the end of the roots. As with root canal treatment it is necessary to follow up to ensure healing proceeds.

ARE THERE ANY ALTERNATIVES TO ROOT CANAL TREATMENT?
When endodontic disease is diagnosed your dentist will outline the possibilities for treatment. These may include keeping a tooth under observation, root canal treatment or extraction. Surgery may also be suggested. If root canal treatment or surgery are not possible or the tooth fails to respond to these treatments, then unfortunately, the only option would be to remove the tooth. If a tooth is lost there are treatments to replace it including implants, dentures and bridges. It should be recognised that although these replacements are available, often retaining your natural tooth is the best choice.
COSTS
If you see a general dentist under the NHS agreement, then they should advise you of the current fee for endodontic treatment. NHS fees for straightforward root canal treatment in England are classified as ‘Band 2’ which is currently £62.10 (differs in Wales and Scotland).
However, if your case is too complicated and falls outside the remit (expertise) for your general dentist then they may have to refer you on a private basis or to a university or NHS dental hospital for further assessment to consider if endodontic treatment is appropriate.
The university will have its own specific criteria on accepting certain cases that are appropriate – usually for teaching purposes. NHS hospital services will be limited to specific criteria for accepting certain endodontic cases based on resources.
If you see a private specialist, they should advise you of the diagnosis, options for treatment, nature of endodontic treatment that they can offer, and their fees.
WHAT HAPPENS AFTER TREATMENT?
Following root canal treatment, you will need a permanent filling. If there is still enough tooth left, then a filling to rebuild the structure of the tooth will be needed, however, if the tooth was significantly broken down then a crown or onlay may be required. These are coverings for the tooth that recreate the original shape of the tooth whilst performing a reinforcing function. Back teeth that are heavily filled and root treated are at risk from fracture if not protected. Sometimes in front teeth, a post may be required to help stabilise a crown. It should be recognised that a filling, crown or other treatment will lead to additional costs.
IS ROOT CANAL TREATMENT SAFE?
There is lots of research that proves root canal treatment is safe and effective. The treatment has a high rate of success, with up to 90% of treatments eliminating disease. There has been much debate and misinformation about endodontic treatment causing ill-health and disease in other parts of the body. This is based on poorly designed research from a century ago and speculation. There is no valid, scientific evidence linking root canal treatment to disease elsewhere in the body. Restoration of endodontic health and saving a tooth, wherever possible, is always the most desirable outcome.
 In conclusion, root canal disease can lead to severe pain and potential tooth loss. It is important to seek the attention of your dentist early so that they can make an appropriate diagnosis and provide treatment to get rid of infection. Although the options for replacement of teeth are advancing continually, there is often nothing better than your natural tooth.
In conclusion, root canal disease can lead to severe pain and potential tooth loss. It is important to seek the attention of your dentist early so that they can make an appropriate diagnosis and provide treatment to get rid of infection. Although the options for replacement of teeth are advancing continually, there is often nothing better than your natural tooth.







